Mako can be used for Total Hip Replacement (THR), which is a procedure designed for patients who suffer from non-inflammatory or inflammatory degenerative joint disease of the hip.
The Mako technology provides the surgeon with a patient-specific 3-D model to pre-plan the patient’s hip replacement. During surgery, the surgeon guides the Stryker robotic-arm based on each patient’s specific plan. This helps the surgeon to focus on removal of diseased bone, helping preserve healthy bone, and assists the surgeon in positioning the total hip implant based on the patient’s anatomy.
Personalized Plan
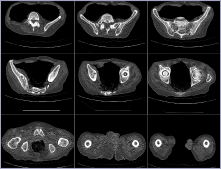
It all begins with a CT scan of the patient’s joint that is used to generate a 3D virtual model of your patient’s unique anatomy. This virtual model is loaded into the Mako system software and is used to create the patient’s personalized preoperative plan.
In the Operating Room
During surgery, the surgeon guides the robotic-arm while preparing the hip socket and positioning the implant based on the patient’s personalized preoperative plan. The Mako system also allows the surgeon to make adjustments to the patient’s plan during surgery as needed. When the surgeon prepares the bone for the implant, the Mako system guides the surgeon within the pre-defined area and helps prevent the surgeon from moving outside the planned boundaries. This helps provide more accurate placement and alignment of the implant to plan.1,2

After Surgery
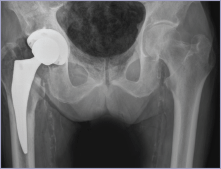
After surgery, the surgeon, nurses and physical therapists will set goals with the patient to get the patient back on the move. They will closely monitor patient’s condition and progress. The surgeon may review an x-ray of the new hip with the patient.
IMPORTANT INFORMATION
Disclaimer
Hip joint replacement is intended for use in individuals with joint disease resulting from degenerative and rheumatoid arthritis, avascular necrosis, fracture of the neck of the femur or functional deformity of the hip.
Knee joint replacement is intended for use in individuals with joint disease resulting from degenerative, rheumatoid and post-traumatic arthritis, and for moderate deformity of the knee. Joint replacement surgery is not appropriate for patients with certain types of infections, any mental or neuromuscular disorder which would create an unacceptable risk of prosthesis instability, prosthesis fixation failure or complications in postoperative care, compromised bone stock, skeletal immaturity, severe instability of the joint, or excessive body weight.
Like any surgery, joint replacement surgery has serious risks which include, but are not limited to, pain, bone fracture, change in the treated leg length (hip), joint stiffness, hip joint fusion, amputation, peripheral neuropathies (nerve damage), circulatory compromise (including deep vein thrombosis (blood clots in the legs)), genitourinary disorders (including kidney failure), gastrointestinal disorders (including paralytic ileus (loss of intestinal digestive movement)), vascular disorders (including thrombus (blood clots), blood loss, or changes in blood pressure or heart rhythm), bronchopulmonary disorders (including emboli, stroke or pneumonia), heart attack, and death.
Implant related risks which may lead to a revision of the implant include dislocation, loosening, fracture, nerve damage, heterotopic bone formation (abnormal bone growth in tissue), wear of the implant, metal sensitivity, soft tissue imbalance, osteolysis (localized progressive bone loss), audible sounds during motion, and reaction to particle debris.
The information presented is for educational purposes only. Speak to your doctor to which therapy is appropriate for you. Individual results vary and not all patients will return to the same activity level. The lifetime of any joint replacement is limited and depends on several factors like patient weight and activity level. Your doctor will counsel you about strategies to potentially prolong the lifetime of the device, including avoiding high-impact activities, such as running, as well as maintaining a healthy weight. It is important to closely follow your physician’s instructions regarding post-surgery activity, treatment and follow-up care.
Speak to your doctor to decide which therapy/treatment is appropriate for you.
Stryker Corporation or its other divisions or other corporate affiliated entities own, use or have applied for the following trademarks or service marks: Mako, Stryker, Together with our customers, we are driven to make healthcare better. All other trademarks are trademarks of their respective owners or holders.
GSNPS-PE-85_17642
REFERENCES
1. Nawabi DH, Conditt MA, Ranawat AS, Dunbar NJ, Jones J, Banks SA, Padgett DE. Haptically guided robotic technology in total hip arthroplasty - a cadaver investigation. Proc Inst Mech Eng H. 2013 Mar22 7(3):302-9
2. Illgen R. Robotic assisted total hip arthroplasty improves accuracy mad clinical outcome compared with manual technique. 44th Annual Advances in Arthroplasty Course. October 7-10, 2014, Cambridge, MA.
